Adam Kleczkowski, University of Strathclyde
Nearly 100 years ago, two British researchers, William Topley and Graham Wilson, were experimenting with bacterial infections in mice. They noticed that individual survival depended on how many of the mice were vaccinated. So the role of the immunity of an individual needed to be distinguished from the immunity of the entire herd.

Fast forward a century and the concept of “herd immunity” is now widely discussed in government dispatches and newspaper articles. But what does it actually mean?
When a disease such as COVID-19 spreads through the population, it leaves some people immune, at least in the short term. The people who become infected later will increasingly have contact with these immune people and not with the susceptible ones. As a result, the risk of infection is reduced and eventually the disease stops spreading. This might happen even if some people in the population are still susceptible.
Vaccination can be used to protect susceptible people and thereby hasten the decline of the epidemic. It can also be used to stop the virus from spreading in the first place.
How does it work?
Imagine a population in which everybody is susceptible. An infected person (the red dot in the chart below) arrives and the virus spreads with the ever-increasing number of new cases. The epidemic continues until most individuals catch the virus and become immune to it or die.
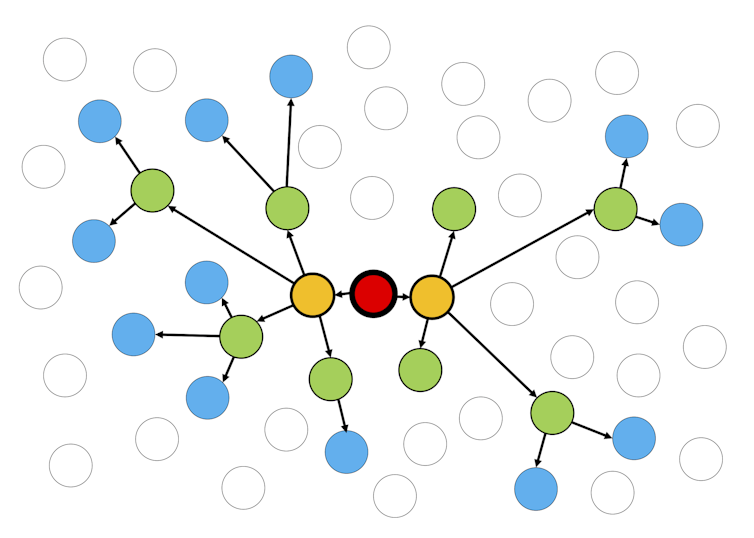
If some people are protected – for example, in the initial stages of a mass vaccination programme – the disease will spread more slowly.
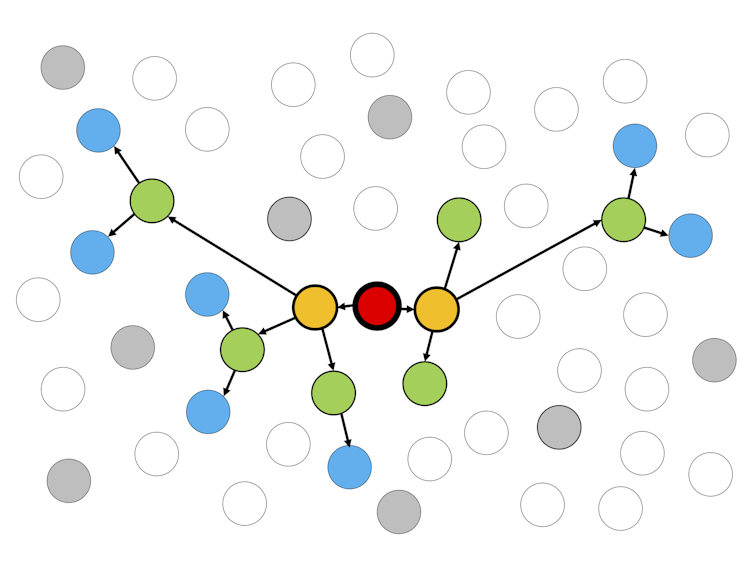
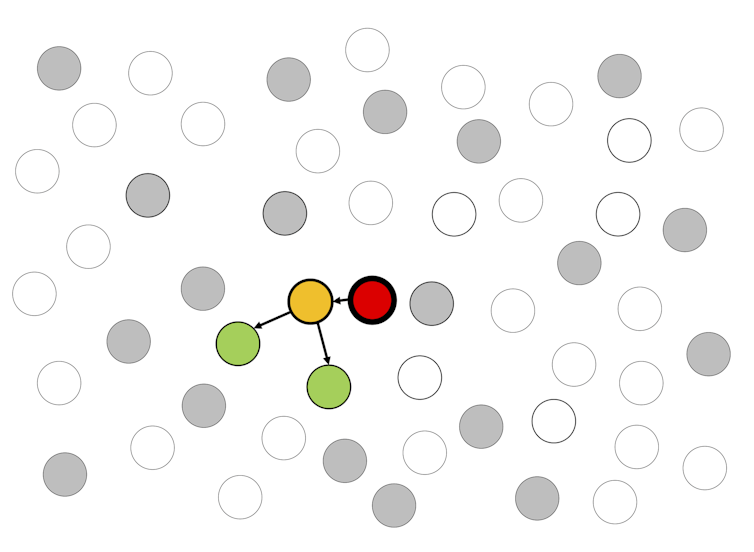
An even more substantial proportion needs to be protected to completely stop the virus, but amazingly it does not need to be the whole population.
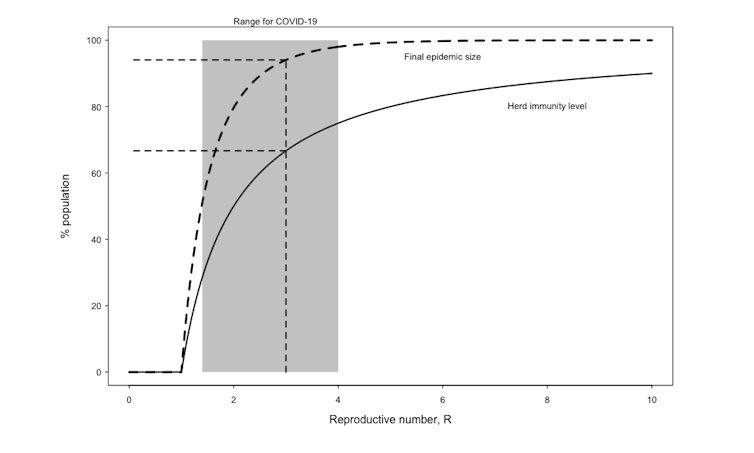
In the 1970s, mathematical epidemiologists found out that this proportion depends on how infectious the disease is, with a simple formula relating it to the reproductive number, R. For measles this critical percentage is 95%, but for influenza, it could be as low as 35%.
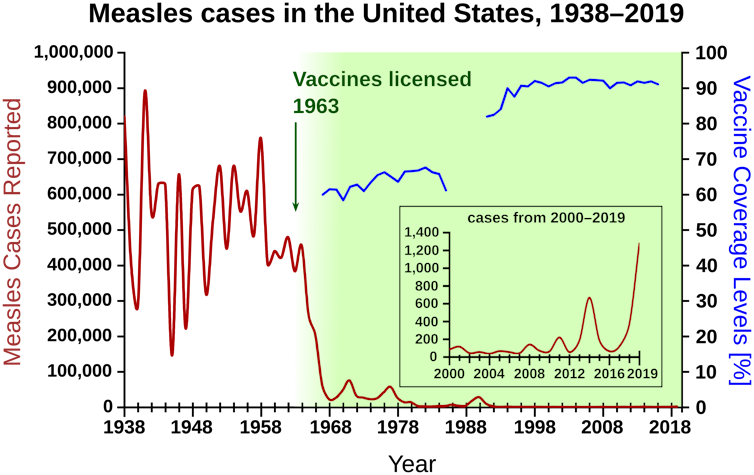
Once the population reaches herd immunity, either through vaccination or naturally by recovering from the disease, any new infection chain will quickly die out. In this way, the population is protected from future outbreaks, but only as long as the immunity levels are maintained.
If the immunity level falls below the critical value, the disease can reemerge. Newborn individuals who are susceptible will need to be vaccinated, and those whose resistance to the disease falls over time might need boosters.
Coronavirus herd immunity
The current estimate of R for COVID-19 is around 3, but is perhaps as low as 1.4 and as high as 4. The corresponding herd immunity level is 60% (50% to 75%).
This value is in the absence of any non-pharmaceutical control measures, such as lockdown. Maintaining some levels of social distancing in the long term allows the desired immunity to be lower while keeping the population safe.
A long time might be needed to eventually eradicate the disease, even after the herd immunity level is reached. So the final size of the epidemic, the number of people who have been through infection when the virus is finally eradicated, can be much higher.
Are we there yet?
It is not easy to determine how close we are to the herd immunity level or whether we will ever reach this stage.
First, the critical assumption is that the coronavirus infection results in a lasting and uniform resistance to future outbreaks. This is far from certain, and if people can catch the SARS-CoV-2 virus more than once, as is the case for the common cold, it will make herd immunity disappear. From large studies to estimate the population immunity, we know that the numbers are currently between 5% and 25%.
Second, the reproductive number, R, varies with location, and so does the herd immunity level needed to stop the disease.
Third, studies suggest that some people have a much higher resistance to COVID-19, perhaps because they suffered from another similar disease in the past or were vaccinated against other diseases.
Finally, there is a large variability in people’s response to the virus and in the length of time for which someone preserves the levels of antibodies they use to fight the infection. The immunity might not be equally distributed among those who have been ill with COVID-19.
People who suffer most might come from the areas that are also most at risk. Such diversity might significantly lower the herd immunity levels needed to stop the disease by targeting only these parts of the society where it is needed most. This phenomenon resembles the ring vaccination strategy that was successfully used to combat such diseases as smallpox.
Individuals or the herd
The concept of herd immunity, although useful for planning a response to the pandemic, is not without controversy. In a campaign to achieve it, many people are exposed to an increased individual risk to protect the rest of the population.
Not imposing strict lockdown measures or relaxing too early might lead to people becoming immune to COVID-19 sooner, reaching herd immunity earlier. But this also leads to excess deaths of vulnerable people who would have survived otherwise.
Herd immunity needs to be maintained. The level required to stop the disease depends on disease transmission, which in turn depends on human behaviour. When faced with potentially grim consequences, our behaviour is naturally to prevent the transmission, which lowers the herd immunity requirement.
Once this is reached, other factors (social, economic, risk of vaccine complications) become more important, transmission increases as a result of behaviour change, and herd immunity is lost. In devising successful strategies, governments must take into account both the population and individual risks and benefits.
Adam Kleczkowski, Professor of Mathematics and Statistics, University of Strathclyde
This article is republished from The Conversation under a Creative Commons license. Read the original article.












