Sarah Pitt, University of Brighton
Following the news that Pfizer’s vaccine for COVID-19 is showing signs of 90% efficacy, there’s been a lot of excitement about the end of the pandemic being in sight. Sir John Bell, regius professor of medicine at the University of Oxford, has even suggested that life could return to normal by spring.

Pfizer’s update certainly is fantastic news. A COVID-19 vaccine could well be approved and ready for use in the next few months. But whether that means we can all get back to normal life by early 2021 is less certain.
If we have a highly effective vaccine that stops people from passing on the virus, and can distribute it worldwide, that would have a massive impact on limiting COVID-19. But we’re probably still a long way from this.
Given we don’t know exactly what effect these early vaccines have, and the logistical challenge of vaccinating billions around the world, it’s more likely the first vaccines will be just some of the tools that we continue to develop to control the coronavirus.
Working with unknowns
The front-running vaccines are all based on getting people’s bodies to produce an artificial form of the virus’s spike protein, which sticks up on its surface and is easy for the immune system to recognise.
These vaccines contain genetic instructions on how to make the spike protein and deliver them to the body’s cells, using either a molecule called mRNA or an altered version of a different, harmless virus. Cells then manufacture copies of the spike protein for the immune system to respond to. Having recognised and remembered what the virus’s outer parts look like, the immune system should then be able to quickly respond to the real virus in the future.
One benefit of this tactic is that it removes the need to expose people to the whole virus when vaccinating them, and so should be safer. It’s also a potentially quicker route to making a safe and effective vaccine when compared with traditional methods that involve using the whole virus.
However, making vaccines that use mRNA or viral vectors is a new field. No vaccines against viral infections based on these methods are in general use yet, so we aren’t sure how good they’ll be.
The interim results for Pfizer’s vaccine – which uses mRNA to deliver its genetic instructions – suggest that it could be highly effective, but there’s still a lot we need to find out. For starters, these aren’t the final results, and it’s important to remember that efficacy in a trial and effectiveness in the real world aren’t necessarily the same. We also don’t know yet if Pfizer’s vaccine actually stops people from transmitting the virus.
If the Pfizer vaccine and the others nearing the end of development all pass their safety and efficacy tests in the next few months, it will definitely be a good idea to try them. But it’s really too soon to tell if they will stop viral transmission in enough people for us to reach herd immunity.
It might be that COVID-19 vaccines based on more tried-and-tested methods – such as Valneva’s, which uses a whole, killed version of the virus – end up being the ones that work best. However, Valneva’s vaccine is not likely to be ready for approval until at least mid-2021.
We also don’t know how long immunity provided by these vaccines will last. We know that antibodies produced after a natural COVID-19 infection can be lost within months. Vaccine-induced antibodies might also fade quickly.
That said, antibodies are probably not the whole answer to the body’s response to this (and indeed other) coronaviruses. Another type of immune response – involving T cells – also seems to be important. Both the Pfizer and AstraZeneca vaccines have shown that they produce a T cell response. But whether these responses are also long lasting is another thing we don’t yet know.
Widespread coverage a challenge
These first COVID-19 vaccines might not be perfect, but let’s say half of the people receiving them make a protective response strong enough to stop them from transmitting the virus. This will certainly help our efforts to control the virus.
But from what we know about SARS-CoV-2, it’s clear that at least 70% of the population will need to have a strong and lasting immune response for the virus to die out altogether. As well as not knowing how long a vaccine-induced immune response might last, there are other factors that will make achieving this a challenge.
Vaccines do not “take” in some people; others cannot be given them due to existing medical conditions. Some people will refuse to be vaccinated.
Achieving 70% coverage will also require mass production to make billions of doses. AstraZeneca has said it has the capacity to produce 2 billion doses of its vaccine, while Moderna says it can have 1 billion doses ready by the end of 2021. Pfizer could have 1.3 billion doses by then – though recipients will need two doses. This leaves us well short of vaccinating enough people.
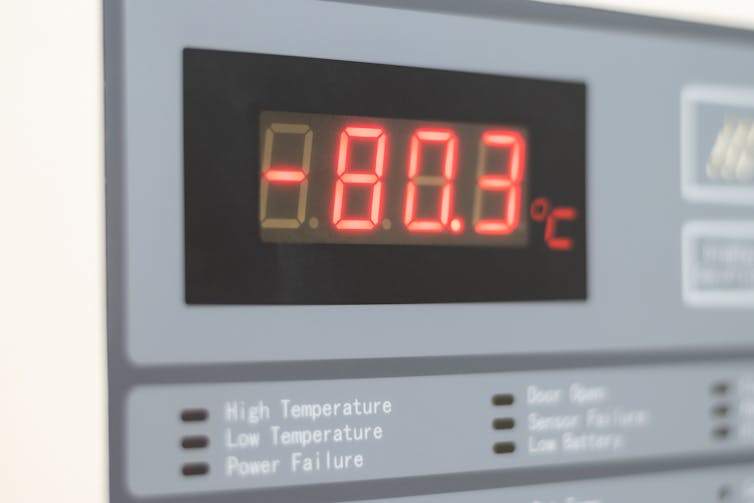
And it will be logistically complex to transport these vaccines across the world and deliver them to all eligible people. The Pfizer vaccine, for example, needs to be kept at -80C. This could prove a challenge even in developed countries, let alone low-resource settings. Rolling out vaccines is definitely going to take more than a couple of months.
All we should really expect from the first vaccines is that they will provide temporary cover to some people. That, of course, will help a bit, but only as part of a suite of measures. We will have to keep up with the social distancing and hand hygiene for a while yet – and expect masks to feature in fashion collections up until at least autumn/winter 2021.
Sarah Pitt, Principal Lecturer, Microbiology and Biomedical Science Practice, Fellow of the Institute of Biomedical Science, University of Brighton
This article is republished from The Conversation under a Creative Commons license. Read the original article.












